If you are a writer, you don’t have to be a masochist to appreciate pain. It’s a great tool for plot, tension, and character traits. I won’t bother defining pain. We all know it when we feel it. Instead, I’ll focus on types, implications, and uses.
Three Pain Anomalies
Any of these can twist the action of your story.
- Experiencing pain in response to a stimulus that is normally painless (allodynia). It has no protective biological function.
- Feeling pain in a part of the body that has been amputated (phantom pain). Actually not so anomalous: it’s experienced by 82%of upper limb and 54% of lower limb amputees.
- Insensitivity to pain stimuli (asymbolia). Indifference to pain present from birth. These people don’t avoid situations/activities that cause pain and bodily damage. Some die before adulthood, all have a reduced life expectancy.
Temporary (Acute) vs. Long-term (Chronic)
Sometimes, the effects aren’t all that different.
- Behavioral deficits caused by being in pain: attention/focus, working memory, mental flexibility, problem solving, and information processing speed
- Use the deficits to ramp up the tension when your hero/ine is trying to achieve a goal
- Use success in spite of these deficits to make your character come across as stronger, more resourceful, more reliable
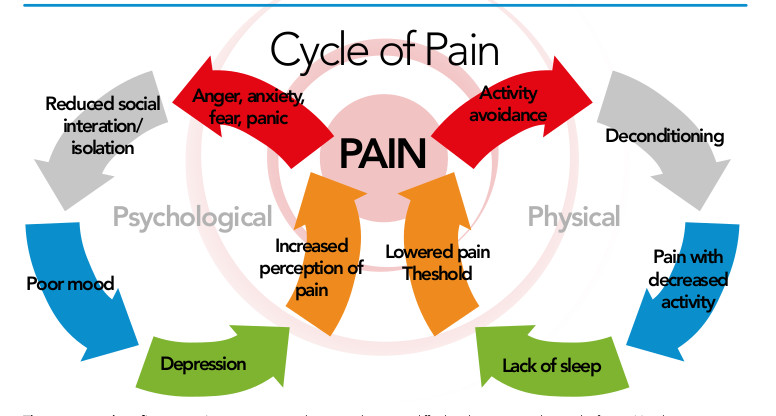
- Intensified negative emotions of depression, anxiety, fear, and anger, when in pain
- Use any of these to create tension between characters
- Use any of these as challenges for the hero/ine to overcome and remain functional
- Following an acute pain episode, people reported feeling better than people who hadn’t been in pain. It feels so good when it stops?

- Chronic pain is associated with several long-term negative side effects:
- Weight gain or loss associated with medications (steroids, nerve pain drugs, opioids) and decreased exercise and activity
- Unpredictable mood swings and increases in scores on tests of hysteria, depression, and hypochondriasis
- Decrease in patience
- Grief for the person s/he once was
- Lifestyle changes:
- Unable to work or provide for family
- Need help to function (get dressed, bathe, eat)
- Loss of prior skill (e.g., can’t play the harp any more)
- Skin, hair and nails can take a beating: increased sensitivity, intermittent spots on face, hair loss
- Intimacy often suffers:
- Sex may be painful
- Ill person may be less energized in finding what works and adapting
- Financial hardship adds to stress, which makes things worth; money goes to medications, lotions and potions, treatments, travel to and from appointments
How to Show Pain When the Character Isn’t Telling
Sometimes, people/characters try to hide their pain. Other times, s/he isn’t able to communicate it. Using these behaviors, you can let the reader or another character know the person is in pain.
- Facial grimacing
- Guarding (trying to protect a body part from being bumped or touched)
- Increase in vocalizations such as sighs or moans
- Changing routines
- Decreased range of motion
- Appearing withdrawn, anxious, depressed, or fearful
- Decrease in social activities
- Decreased appetite
- Increases in confusion or display of aggression or agitation
- Decline in self-care
- Side effects from hidden medication
- Over-the-counter pain medication often causes stomach irritation and nausea; people taking these medications may uncharacteristically refuse alcohol
- Prescription pain medication, even when taken responsibly, often cause random itching, slowed breathing, constipation, and nausea; drowsiness and confused thinking (agitation, euphoria, etc.) are probably the most noticeable side effects
Why Would Someone Want to Hide Pain?

- Don’t want to look weak
- Showing pain is impolite
- Showing pain is shameful
- Pain is seen as a deserved punishment
- Pain was self-inflicted as a maladaptive coping mechanism
- To avoid treatments against one’s religious beliefs
- Afraid it means death is near
- To avoid treatment that might lead to addiction
- Don’t want to admit needing help
- To avoid being disqualified from certain careers or activities
- To shield another character from the knowledge
- Showing pain would lead to more pain being inflicted
Gender and Pain
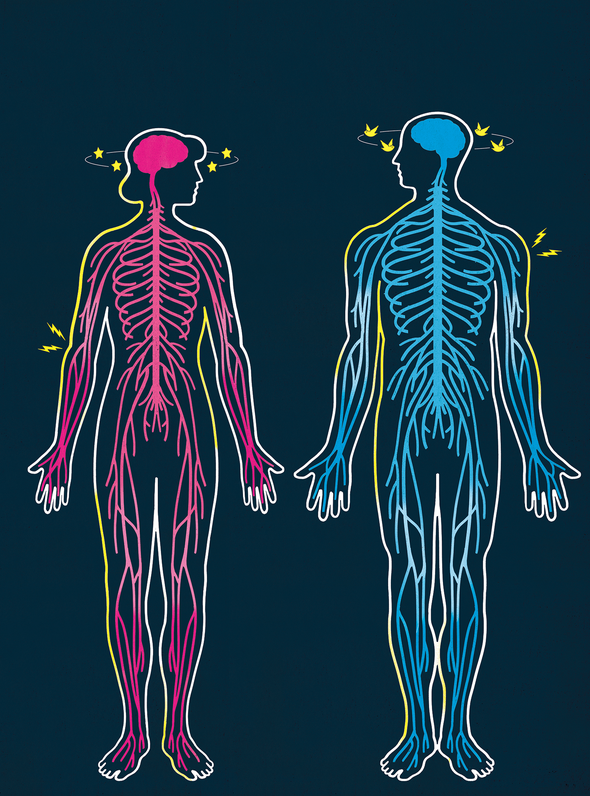
- Socially and culturally, acknowledging pain is more acceptable for women than for me. Women are expected to be emotional, men stoic.
- Female pain is often stigmatized, leading to less urgent treatment, longer wait times in emergency rooms, and doubting the accuracy of women’s reports of pain.
- Statistically, women are more likely to be prescribed sedatives for pain; men are more likely to be prescribed actual painkillers.
- Study shows men more prone to hypersensitivity when exposed to an environment in which they remembered feeling pain.

Beauty Knows No Pain

Many activities require some amount of pain, if only at the beginning. Lifting weights, running, bicycling, and other workout routines can cause severe soreness and muscle aches the first few times a character exercises. What would make a character get up and do it again? Training to compete in a sport is likely to cause some pain as the human body is pushed beyond its previous limit. How much is too much, enough to make a character quit?

Developing the callouses necessary for manual labor, martial arts, playing stringed instruments, some types of dancing, etc. almost always involves blisters and bleeding along the way. Some activities always involve some level of pain, such as dancing en pointe, Tough Mudder runs, or boxing. What might make a character work past the pain to perform any of these? How might characters convince themselves to repeat the necessary movements, knowing how much they will hurt?

Beauty and fashion often come with pain of their own: tattoos, corsets, high heels, neckties, piercings, trendy clothes too hot or too cold for the environment… Why? Consider the different standards of beauty at different time periods or in various cultures; how much pain would a character be willing to undergo to achieve these standards?
Describing Pain More Vividly

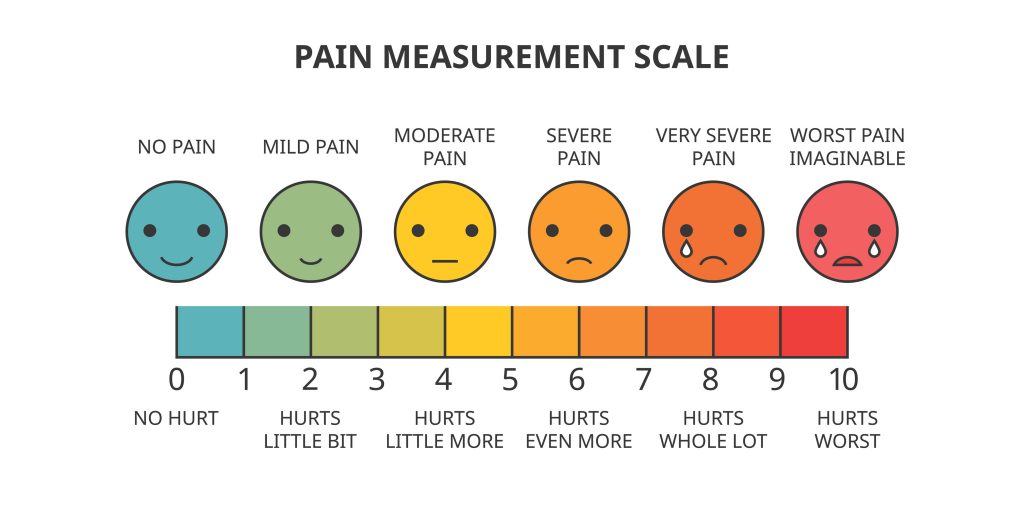
Be precise about location, intensity, whether it’s continuous or intermittent, whether it’s burning, sharp, deep or superficial, diffuse or focused. In a medical environment, patients are often asked whether their pain is new (acute) or ongoing (chronic). There is a difference between shooting pain and stabbing pain; there is a difference between a stomachache and a pressure ache in the upper, right abdomen. Pain in ligaments, tendons, bones, blood vessels, fasciae, and muscles is dull, aching, poorly-localized. For example, sprains and broken bones are felt as deep pains. Minor wounds and burns are superficial. Is this pain burning, tingling, electrical, stabbing, pins-and-needles? Further examples of pain descriptors can be found here or here.
Give That Baby Sugar?

Fun tidbit: sugar taken by mouth reduces pain in newborns resulting from lancing of the heel, venipuncture, and intramuscular injections. It does not remove pain of circumcision. The reduced pain of injections might last till age 12 months. Mary Poppins was right: a spoonful of sugar really does help the medicine go down!
Bottom line for writers: pain is incredibly useful in numerous ways.