People typically feel relaxed and calm when they do things that stimulate the parasympathetic nervous system, allowing them to let go of tension and stress. When the bad vibes threaten to overwhelm you, consider the following suggestions to return good vibes to your life!
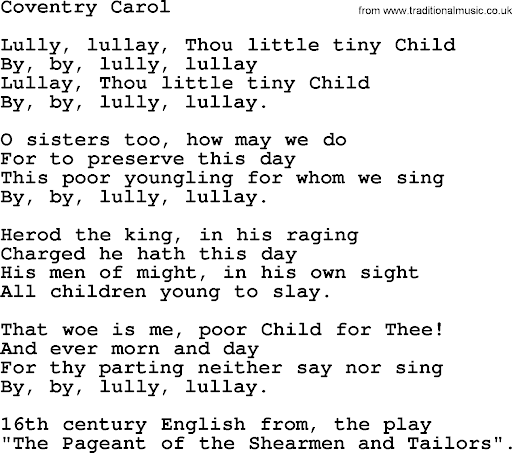
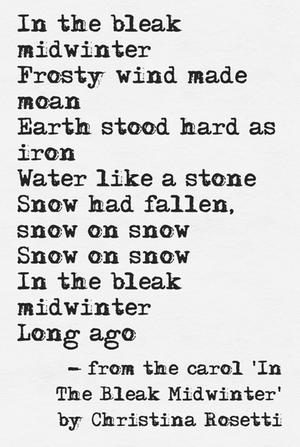
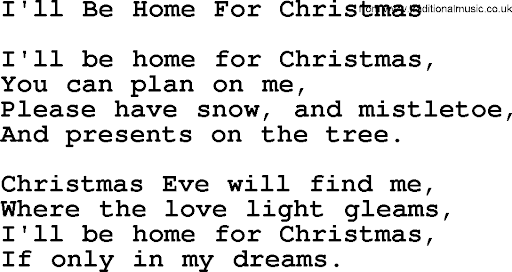
Sounds Can Promote Relaxation
Listening to calming music can promote good vibes. Such music typically features slow, soothing melodies, minimal percussion, and soft instrumentation such as piano, guitar, and strings. The tempo is generally slow, and the volume is often kept low to create a peaceful atmosphere.
Nature sounds, such as ocean waves or rain, rustling leaves, chirring of insects.
Gentle ambient noise, such as a fan or “noise machine.”
Sights
If you feel the craziness closing in, your eyes can help restore your good vibes!
Water is key: Looking at water, especially calm bodies like a lake or a quiet ocean, can significantly lower heart rate and blood pressure, inducing a meditative state.
Natural patterns: Fractal patterns found in nature, like the branching of trees or the ripples on water, can be particularly soothing.
Wide open spaces: Expansive landscapes with open horizons can promote a sense of peace and tranquility.
Activities
There are steps you can take to improve the vibes in your life, some easier than others.
Deep breathing: Focusing on slow, deep breaths is a highly effective way to activate the relaxation response in the body. It’s a simple and effective way to reduce anxiety and anger.
Heat: Taking a warm bath or applying heat to tense muscles can induce relaxation.
Physical activity with low intensity: Gentle stretching, yoga, or walking can help release tension in the body.
Get into nature. Nature is calming because it provides a sensory experience that engages multiple senses with sights, sounds, and smells that are often repetitive and predictable, which can help to reduce stress, lower heart rate, and promote relaxation. Being in nature essentially acts as a distraction from daily worries and allows for a sense of connection to something larger than oneself. Many of these benefits come to gardeners. There is also something called the biophilia hypothesis: research suggests humans have an innate connection to nature, which can lead to feelings of well-being when exposed to natural elements.
Keep a journal. It provides a safe place to express and process your thoughts and emotions, allowing you to gain clarity, release pent-up feelings, and reflect on experiences, often leading to a sense of reduced stress and anxiety.
Get creative. Creativity often leads to a sense of self-expression, reduced stress, and a feeling of control over your inner world, essentially providing an outlet to process and release tension. Creativity can put us in a flow state, meaning we become focused with optimal attention on a task or activity. This is sometimes called being “in the zone.” When we are in the zone, it can feel euphoric, and we become more mindful and relaxed.
Mind Games
The phrase “mind games” tends to evoke images of power-hungry bosses or abusive ex-partners. However, you can also play mind games with yourself to encourage healthy practices!
Mindfulness practices: Meditation and other mindfulness techniques help to quiet the mind and become more aware of the present moment, reducing stress.
Relaxing imagery: Can help calm down angry feelings.
Being grateful: Practicing gratitude can reduce cortisol, the key stress hormone. You can record your gratefulness in a journal.
Visual imagery: Imagining peaceful scenes or calming scenarios can help to distract from worries and promote relaxation.
Environment
The outside impacts the inside. By the same token, surrounding yourself with good vibes has a powerful impact on mental well-being.
Warm environments are more relaxing than cold ones.
Color palette: Soft, muted colors like blues, greens, and pastel shades are generally considered calming.
Limit clutter in your personal environment.
Limit your exposure to negative stimuli, such as disturbing news.
Habits
On their own, small habits may not make much difference. But when you practice them regularly, you may find an appreciable improvement.
Regularly engage in positive social interaction: Spending time with loved ones or engaging in pleasant conversations can promote feelings of well-being and reduce stress.
Sleep: Getting enough sleep is important for thinking clearly and controlling negative emotions. To sleep better, you can avoid caffeine, alcohol, and heavy meals before bed.
Nutrition: Eating well is a key part of maintaining calm. See below.
Physical activity: Exercise can help you feel calmer.
Routines: Having a consistent morning routine can reduce decision-making and stress.
Eating and drinking
What you put into your body can have a major impact on how your brain works. Nutritionists have identified many foods that support mental health and well-being.
Lots of people relax with alcohol, but this is not a good primary practice, given the empty calories, loss of control, and potential for addiction.
Instead limit caffeine and drink chamomile tea and green tea.
Complex carbohydrates are good, including whole grains like breads and pastas, brown or wild rice, and oatmeal.
Omega-3 fatty acids, found in fish like salmon, tuna, and halibut; avocados; flaxseed.
Magnesium from foods such as leafy greens like spinach and Swiss chard; legumes, nuts, and seeds; dark chocolate; bananas.
Vitamin C is good, from berries like strawberries, raspberries, blueberries, and blackberries; and, of course, oranges.
Surprise! You can get probiotics from pickles, sauerkraut, and kefir.
Other good foods: yogurt, dark leafy greens, asparagus, oysters, cashews, liver, beef, and egg yolks.
You can also try eating lean proteins to help calm you.
Emotional Control
The physical environment can certainly influence good vibes, but exercising emotional control can have a powerful effect on mental health.
Treat yourself kindly: Calm people don’t beat themselves up about mistakes or weaknesses.
Seeing the middle ground: Expect that there will be glitches, even when people do their best.
Respecting boundaries: Setting boundaries can lead to long-term benefits.
Use your phone judiciously. Be mindful about media you consume.
Why Bother?
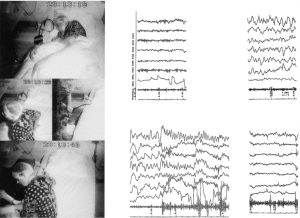
Regular practice of relaxation techniques will assist you in relieving muscle tension, reducing anxiety, and improving your overall wellbeing.
Other physiological benefits:
- Decrease in heart rate
- Decrease in respiration rate
Being calm and relaxed significantly improves both mental and physical health:
- Reducing stress
- Lowering blood pressure
- Enhancing focus
- Improving sleep quality
- Boosting mood
- Allowing for better decision-making, ultimately leading to a higher quality of life
Essentially, it allows your body and mind to recharge and function optimally.
Bottom Line: There are myriad ways to relax and promote calm, and the benefits are well worth the effort.