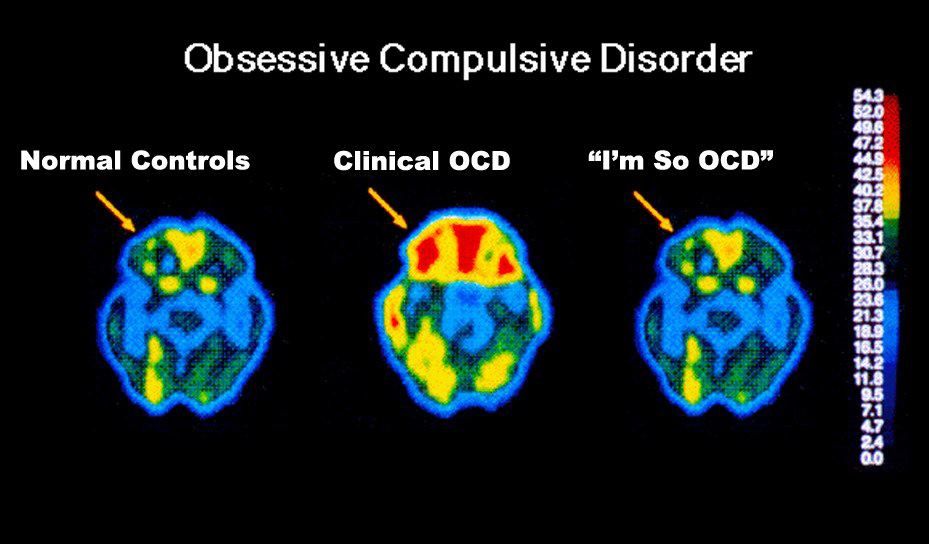
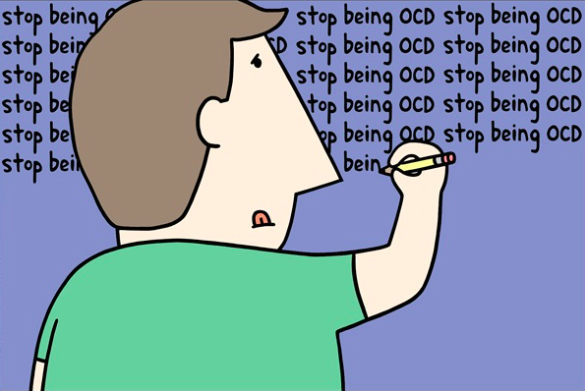
OCD, like love and hate, is a label thrown around pretty loosely, often for humorous effect. People with fixations on organization, precise routines, hygiene, perfectionism, etc. are frequently referred to as “acting so OCD” or “showing their inner OCD.” Marketing campaigns turn OCD into a punchline to sell products like Obsessive Christmas Disorder pajamas or Khlo-CD organizational apps.

There is a significant difference between people with odd quirks and people who have a diagnosable mental illness. Both can be useful characters for writers, albeit in very different ways. Characters who have fixations, quirks, rituals, or habits that interrupt a scene or cause awkward situations can be a source of amusement for writers. Characters who actually have Obsessive Compulsive Disorder can be a source of tension, tragedy, or demonstrated compassion for writers, but the actual mental illness is not amusing.

Obsessive-Compulsive Disorder is a common, chronic, and long-lasting disorder in which a person has uncontrollable, recurring thoughts (obsessions) and/or behaviors (compulsions that s/he feels the urge to repeat over and over). The line between having a personality quirks and a mental disorder can be hard to find, but it generally comes down to quality of life. Dr. Steven Brodsky points out that actual OCD will “impair social or occupational function or involve frequent excessive distress” in the lives of those suffering from it.

- Obsessions—repeated thoughts, urges, or mental images—are private, and thus no one knows about them but the person unless they’re talked about. These uncomfortable thoughts cause anxiety.
- Compulsions are typically (but not always) public, as is any behavior that happens the presence of others. The repetitive behaviors are an attempt to deal with the anxiety the obsessive thoughts create.
Could you benefit from an O and/or C character? Although people/characters can exhibit symptoms of obsessions, compulsions, or both, thoughts and behaviors typically occur together. See the end of this blog for specific prompts.

Consider Monk, The Big Bang Theory, and Friends. All three shows feature characters who exhibit signs of obsessions and compulsive behaviors, usually to the sound of the laugh-track. All three characters are referred to by others as “obsessive,” “OCD,” or some variation thereof, but none experience the pain that comes along with mental illness (which I can only imagine would be heightened by hearing laughing crowds).
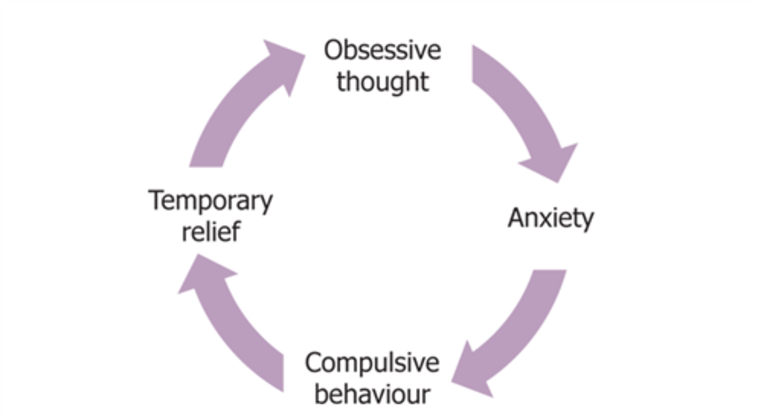
Obsessive thoughts and compulsive behaviors become part of a vicious cycle in the minds of people with OCD. Most people with OCD realize that their thoughts and behaviors are irrational, but they are unable to break the cycle. Children often don’t perceive their abnormality; symptoms are noticed by parents and/or teachers.
In contrast, “neat freaks” and people with fixations often enjoy performing the behavior in question (such as alphabetizing books), enjoy the results (such as having a tidy apartment), have had the behavior drummed into them (such as rewinding video tapes after working at Blockbuster for years [I realize that I’m dating myself]), or out of practical necessity.

Most People with OCD Fall Into One of the Following Categories (in no particular order)

- Washers are afraid of contamination. They usually have cleaning or hand-washing compulsions. Many refuse to wear anything someone else has worn, take their own sheets to hotels/motels, etc.
- Washing your hands before and after eating is just being extra hygienic; washing your hands until they are raw and cracked is a probable sign of OCD.
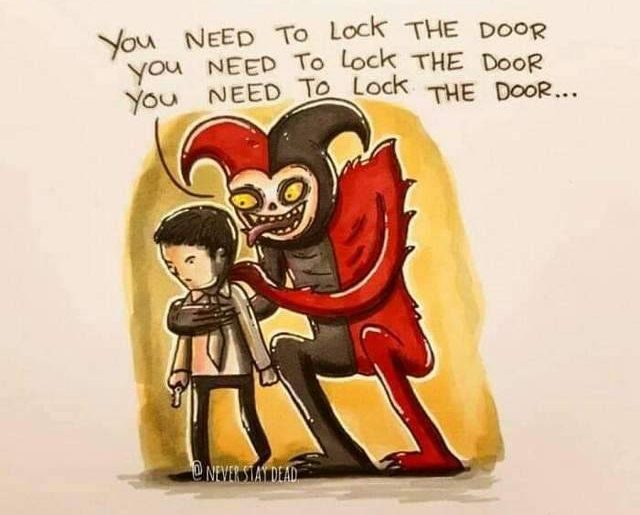
- Checkers repeatedly check things (motion-sensor lights turned on, car locked) they associate with safety. They might keep guns or other weapons that are checked for accessibility, condition, etc.
- Jiggling the door handle after locking it could be a funny quirk; checking the lights, the thermostat, the window latches, and everything else repeatedly until you’re late for work is a sign of unhealthy compulsion.

- Doubters and sinners are afraid that if everything isn’t perfect or done just so something terrible will happen or they will be punished. Dressing, undressing, bathing, eating must be done in precisely the same way, for example. Or furniture cannot be moved. Cars must always be the same make.
- This can also take the form of rituals that must be completed regardless of convenience or safety, such as always taking seven steps at a time or touching every surface in a room, including the hot stove top.

- Counters and arrangers are obsessed with order and symmetry, perhaps including superstitions about certain numbers, colors, or arrangements. For example, counting all the angles in a room, or the number of furniture legs.
- Being unable to enter rooms painted blue or walk without counting sets of four steps sounds amusing… until the door out of the burning house is in a blue room five steps away.

- Hoarders keep things they neither need nor use. They fear that getting rid of anything will cause something bad to happen, or it will be needed later. These people are often co-diagnosed with other disorders, such as depression, PTSD, ADHD, compulsive buying, or kleptomania. They might engage in skin-picking.
OCD symptoms may come and go over time. Added stressors increase symptoms.
It’s a vicious circle: obsessive thoughts trigger anxiety, which leads to compulsive behavior to try to curb the anxiety, and the behavior is followed by temporary relief.
Writers consider the following:
- A person who actually is threatened in some way while others dismiss the anxiety and precautions as being silly fixations
- A character whose compulsive behaviors are humorous and the source of derision/ joking among coworkers or friends/ acquaintances
- A character whose compulsive behaviors embarrass children or other family members
- A person whose compulsive behaviors put the family in financial jeopardy
- A person whose compulsive behavior leads neighbors, classmates, and others to ostracize the person AND his/her family
- A character who keeps obsessive thoughts private, doesn’t act on them, and the strain leads to withdrawal from intimate relationships
- A character whose obsessions get them into medical or legal trouble
- A character whose OCD has become so severe that they are unable to leave the house or keep a job

Bottom line for writers: OCD characters can provide tension, tragedy, and plot development; fixated or quirky characters can provide humor. There is a big difference.