Stress and alcohol go together like peanut butter and jelly—a burger and fries, mac and cheese, bread and butter, mashed potatoes and gravy, milk and cookies, or any other iconic duo you can think of. Yes, they can be separated but—oh, so often—you don’t have one without the other.

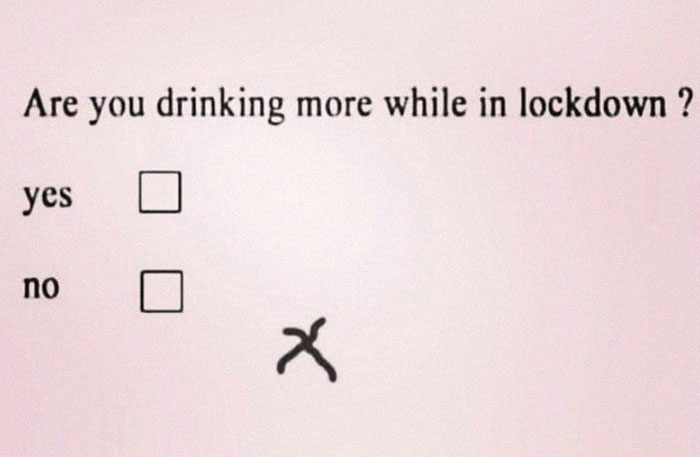
I started thinking about this when the Richmond Times-Dispatch ran a front page story (above the fold!) about liquor sales in Virginia. You will recall that ABC Stores have remained open as “essential” services. And according to numbers from the Virginia Alcoholic Beverage Control Authority, sales now hover around $22 million a week.
In March, as the social distancing began, the ABC stores had more than $30 million per week. Sales in April 2020 were up about 15% over a year ago. The article goes on to identify the top selling brands for the state and for the Richmond Planning District (City of Richmond, Henrico, Goochland, Hanover, Chesterfield, and Powhatan counties). I was less interested in the rankings than in the sheer volume!
Alcohol consumption is up all over the country. To look at one other location, in Tulsa, OK, one liquor store reported that looking at sales March 15 to April 15, liquor sales were up 56% and beer 48%. Compared to a similar date in April of 2019, one-day sales in April 2020 were up by 100%.
According to one store owner, buying habits are changing in that people are buying more at a time, shopping more during the day and less in the evenings and on weekends.
In order to facilitate buying alcohol, providers are offering digital ordering and delivery, curbside pick-up, hosting, hosting virtual tastings and/or cocktail hours. And some are branching out by stocking hand sanitizers and face masks. Virtual cocktail parties among friends and families are now common.

Estimates of the increase in U.S. alcohol consumption from now to the same time last year vary from 25% (WHO) to 55% (Healthcare Home [//healthcare.utah.edu]).
The uptick in alcohol consumption is not solely a U.S. phenomenon. The World Health Organization has issued statements urging countries world-wide to try to curb drinking during the current pandemic. They cite several health reasons to try to control excessive alcohol consumption. No matter how bad a situation is, excess drinking can always make it worse!

- Weaken the immune system, actually making people more vulnerable to infection
- Exacerbate existing health problems
- Increase risk-taking
- Increase violence (“a horrifying global surge in domestic violence”)
- As victims of domestic abuse find themselves trapped at home under constant surveillance by their abuser, many have trouble accessing resources. Some organizations are offering discreet assistance for people with no physical or virtual privacy.
- Circle of 6
- One Love Foundation
- Private sellers of make-up or beauty products who will not be listed here as that would defeat their anonymity
- The National Domestic Violence Hotline (1-800-799-7233), Futures Without Violence, National Network to End Domestic Violence, National Coalition Against Domestic Violence, Stronghearts Native Helpline (1−844-762-8483) and other organizations provide more information about available resources during the pandemic.
- As victims of domestic abuse find themselves trapped at home under constant surveillance by their abuser, many have trouble accessing resources. Some organizations are offering discreet assistance for people with no physical or virtual privacy.

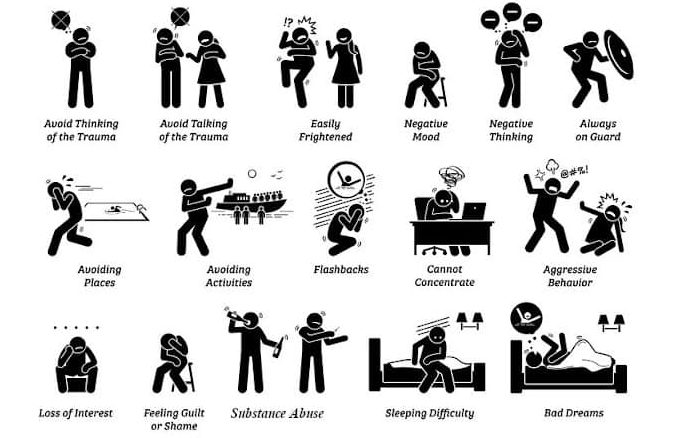
- Contribute to or worsen mental health problems
- If you are in a crisis, please call (1-800-273-8255).
- The Suicide Prevention Lifeline, Zero Suicide, the Suicide Prevention Resource Center, and the National Alliance on Mental Illness have all updated their websites with information about mental health assistance during the pandemic.
Also according to WHO, alcohol-related deaths number 3 million every year—before the pandemic. And the WHO now has the added difficulty of trying to quash the misinformation that has circulated to the effect that drinking can make someone immune to the COVID-19 virus and/or cure one if infected. The presumed medicinal value of alcohol has a long history (see below), perhaps with roots in the dulling of physical pain.


The link between stress and alcohol consumption is so well established that it’s actually called “self-medication.” In fact, such self-medication can be pretty effective, at least initially, in relieving anxiety and depression. Alcohol is a “downer” (i.e., a system depressant) so if people are wound up, rapid heart beat, etc., alcohol can definitely make those symptoms of stress go down. But as mentioned above, alcohol also depresses inhibitions, increases risk-taking, decreases logical decision making, increases violence, and — after all that — is still likely to interfere with restful sleep.

COVID-19 presents a set of circumstances that are problematic with regard to alcohol consumption.
- High levels of anxiety associated with the unknown
- Isolation from one’s usual support system
- Loneliness
- Economic distress/job loss
- Food insecurity
- Fear of infection/death
- Mourning the loss of a loved one
- Stress at having to work from home
- Stress of having to work in an “essential” job interacting with the public
COVID-19 is dominating today’s headlines, but it is far from unique. Research indicates that alcohol use and abuse increase during and after “violent conflicts”—e.g., wars, periods of martial law, government coups. Other psychotropic substances are also used to deal with psychic strains and trauma, but alcohol is generally the most likely to be readily available, legal, and (at least within limits) socially acceptable.
During the 1918 Influenza Pandemic, bootleg whiskey was viewed as a respectable medicine. At the time, more than half the states in the U.S. had passed Prohibition laws and thus were “dry.” But for medicinal purposes, some officials decided to tap the vast stores of liquor that had been confiscated initially to aid the military, although the Army mostly remained silent about using it. In Richmond, Virginia—reportedly—two railroad cars of confiscated whiskey arrived for the benefit of Camp Lee. Over time, confiscated whiskey was distributed to civilian hospitals, too.

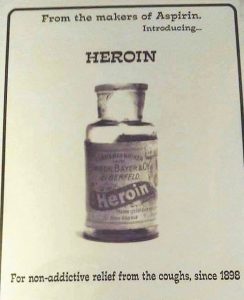
The United States Pharmacopeia dropped whiskey, brandy, and wine from its listing of therapeutics in 1916. In 1917, the American Medical Association resolved that “the use of alcohol as a therapeutic agent should be discouraged.” Even so, more than half of physicians believed it was “a necessary therapeutic agent.” It continued to be available by prescription in dry states. To this day, strong alcohol is prescribed for medicinal purposes in some areas, even by doctors!
Besides the demand for alcohol, the Spanish Flu pandemic shared other characteristics with COVID-19:

- Wearing masks
- Social isolation
- Use of disinfectants
- Limiting group gatherings, including churches
- Hospitals and funeral homes were overwhelmed
- During Spanish Flu the treatment of choice was aspirin, up to 30 grams daily which is a toxic dose; currently, think ingesting bleach or disinfectants.

Bottom line for writers: people use alcohol to self-medicate for stress. The current stressor is COVID-19 BUT consider all the other stressors out there, which might occur alone or in combination with COVID-19: death of a loved one, job loss, divorce, physical illness, mental illness, physical disability, too little money, going hungry, being homeless… Do you have a character who does—who could—self-medicate with alcohol?